Dental implants can come in many different shapes, sizes and materials. Depending on the right fit for the patient, the dental implant design and materials used can vary. Allergies, aesthetics, patient preference, and how the teeth bite together can influence the materials that are chosen for the entire dental implant.
Dental implant posts that are inserted into the jawbone are made out of titanium, titanium alloys, and zirconia, which is a newer implant design. Dental implant crowns can be made out of porcelain fused to metal, zirconia (minimizes gray gumline), e-max and gold.
Dental implants are ever-evolving and have come a long way since they first started to be done to replace lost or missing teeth. More and more research is being done to figure out what materials work best and how to make the implants look the most aesthetically pleasing.
Sometimes we can look at a person’s smile and immediately pick up on the fact that their smile is not completely natural. Not that that’s a bad thing, but I know most people would rather a smile that is aesthetically pleasing, without sticking out. I mean, that’s why dental implants are chosen for treatments because they resemble a natural tooth the most out of other tooth replacement options.
In this post, I go over more materials that are used, not just the ones used for the implant posts and crowns. Dental implant posts are connected to the crown by an abutment, and the crowns can either be attached to it by a screw or cement. As well, I touch on the different implant treatments and implant maintenance.
What dental implants are made of
Why does the material of the dental implant matter? And why can’t we just use anything? The body is an intricate being, and materials need to be both functional, structural and coexist with our body. Being biocompatible is completely necessary when exploring different materials to be used in dental implants.
The reason why biocompatible materials are so important comes down to how the implant attaches to both the bone tissue and the gum tissue.
How the gum and bone tissue attach around the implant differ from natural teeth. The gum and bone tissue around natural teeth adhere to the tooth by little ligaments called periodontal ligaments.
Visualize a trampoline, and picture all the springs that attach the frame to the trampoline mat. Imagine your tooth is the trampoline mat, being held in place by springs.

The springs allow for movement of the teeth, and keeps the tooth in the socket.
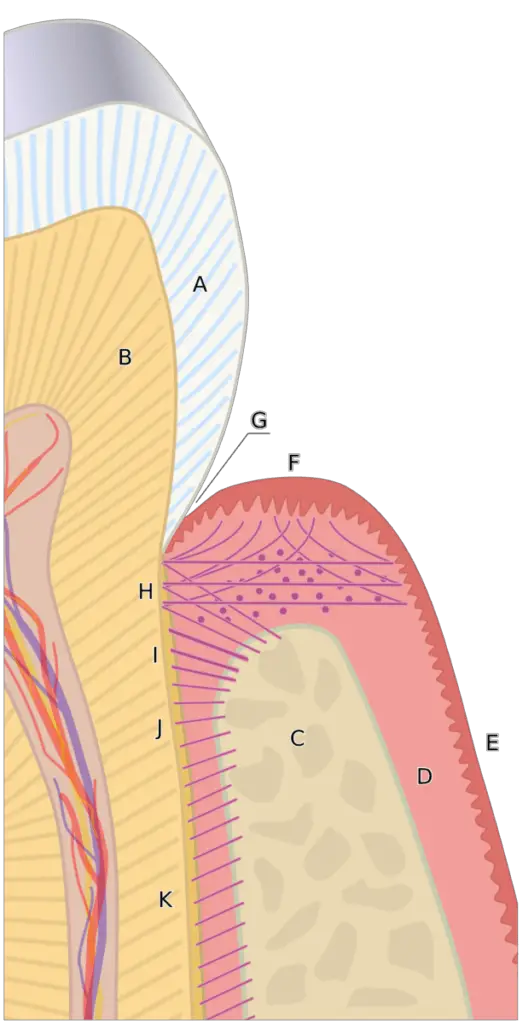
So how does a dental implant stay in place? There are no “springs” to hold it in place.
The implant holds its place by integrating directly into the bone tissue, called osseointegration. And only certain materials can osseointegrate into the bone tissue of our bodies and be completely biocompatible.
A dental implant consists of 3 different components. The implant post goes directly into the jaw bone, the abutment attaches to the implant post, and the crown is attached to the implant abutment. Each component of the dental implant can be made out of different materials.

A few implant post material options exist, that can effectively osseointegrate with the bone. These materials are:
- Titanium
- Titanium alloys
- Zirconia
Implant abutments can be made out of a few more materials:
- Titanium
- Titanium alloys
- Zirconia
- E-max
- Alumina
Implant crowns have a few more options for what they can be made out of. These materials are:
- Porcelain
- Porcelain fused to metal
- Zirconia (minimizes gray gumline)
- E-max
- Gold
Factors determining implant crown material
Choosing the right material for the implant crown relies on so many factors. What material being used will be discussed between the patient and the dental professional, going over the patient’s personal needs and wants, along with what will be both the most functional and aesthetic.
The biggest factor that impacts the material used for implant crowns is durability. Does the patient have a really hard bite? How much room is there between the teeth, how is the implant crown angled?
Some implant crown materials are quite soft, and others are harder and more durable. Each of the materials comes with there aesthetics, and how they look can be extremely personal for the patients.
Dental implant prosthesis options
Single-tooth replacement

This treatment is used to replace one missing or lost tooth. A single-tooth replacement consists of one implant post and one implant crown.
Dental implant bridge
This treatment is used to replace multiple missing teeth in one area of the mouth. Usually, this treatment replaces 3 teeth but could extend to more teeth, using more implant posts. A dental implant bridge usually consists of 2 implant posts, and 3 crowns all fused together.
All-on-four denture implant prosthesis

This treatment is done instead of having traditional dentures. Traditional dentures are known for “floating” on top of the gum tissue, becoming loose, and make eating difficult.
All on four is a great way for dentures to stay in place, and preserve some of the bone tissue. Some can be removed so the dentures can be cleaned properly, being soaked, as well as making it easier to clean the part of the implant the extends up through the gum tissue.
All on four implants usually use 4 implant posts in the jaw and a denture will clip into the implants, securing it in place.
How are the implant crowns attached to the implant?
Cement-retained implant crowns
Cement-retained implant crowns are the most common way of attaching the crown to the implant. Cementing can provide more room for error when placing the crown, however, there are larger risks that come along with cement-retained implant crowns.
The biggest issue with cement-retained crowns is the cement. It is extremely difficult to ensure that all the excess cement is removed before it hardens. Excess cement – even a microscopic amount, increases the risk of peri-implantitis (bone loss and inflammation around the implant).
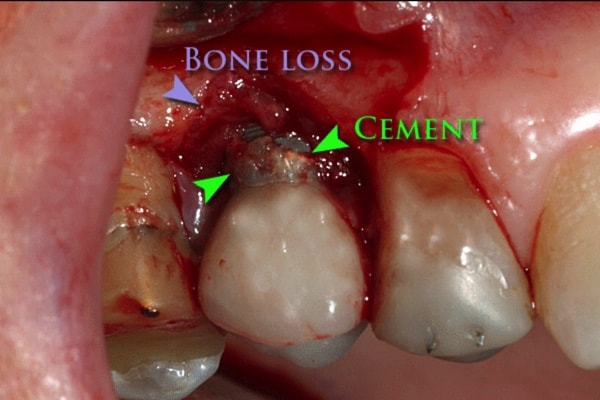
Peri-implantitis is a chronic inflammation of both the gum tissue and the bone tissue around the implant, which can lead to bone loss and failure of the implant.
I have had a few patients who have cement-retained implant crowns, and their oral hygiene is incredible. However, due to the cement, they have ongoing chronic issues around the implants. And even one of my patients ended up losing multiple implants because the cement caused excessive bone loss.
Also, if something were to happen to the implant, and the crown needed to be taken off, it is much harder to remove a cement-retained crown than it is to remove a screw-retained crown.
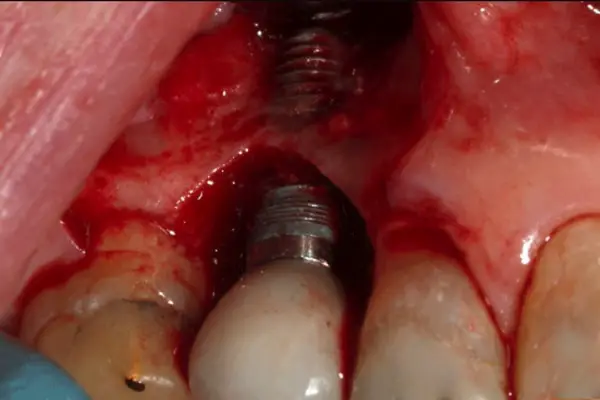
Screw-retained implant crowns
If I were to ever get an implant, I would opt for a screw-retained implant crown if it were feasible.
Within the implant crown, there is a hole that the screw goes into, and it connects to the implant abutment/post. Once the crown is screwed on, filling material is placed on top of the screw to seal it and make a smooth top of the tooth.
For any reason that the crown needs to be taken off, screw-retained implant crowns are much easier to take off than cement-retained crowns.
Are cement-retained or screw-retained implant crowns better?

Screw-retained implant crowns are recommended whenever possible. According to this documen t, cement-retain implant crowns should only be done if the margin is above the gum line, or the crown is really narrow and a screw would not fit.
t, cement-retain implant crowns should only be done if the margin is above the gum line, or the crown is really narrow and a screw would not fit.
Maintaining dental implants

Having dental implants last for a long time is the ideal especially considering the expense of them. However, they need to be taken care of to prevent them from failing. Gum disease can progress faster in dental implants, and once they start to fail, it can be difficult to make the tissue around them healthy again.
Being consistent with flossing, brushing, using a Waterpik, and using other oral hygiene devices helps to prevent inflammation that can cause the implant to fail.
I put together a couple of different resources to guide you on the best ways and tools to clean the dental implant properly. I have linked to them below.
Dental Implants and How to Take Care of Them After Surgery
Cleaning Under Your Dental Bridge Made Easy: With Pictures
Holly 🙂