
Currently, in my dental hygiene practice, I see mostly adults and elderly patients, with many who’ve had some form of bone loss in their jaw. Often when I am discussing bone loss with my patients, a common question I get is; Can the bone loss in their jaw be reversed?
Bone loss in the jawbone cannot be reversed but can be stopped from progressing further with frequent dental hygiene therapy and at-home care. Oral surgeons can perform flap surgery to reduce the periodontal pockets to increase the success of maintaining bone levels and prevent tooth loss.
Losing the bone in the jaw and surrounding the teeth can lead to complications, and make oral hygiene more difficult, leading to a higher incidence of cavities and progressing gum disease.
In this post, I further explain why bone loss cannot be reversed, how fast bone loss can occur, causes of bone loss, treatment options and advice that I give my patients in my dental chair!
Why bone loss in the jaw cannot be reversed
The most common reason for bone loss in the jaw is gum disease. Gum disease affects half of Americans over the age of 30! That’s a huge number! And a lot of them probably don’t even know they have it. That is why seeing a dental professional regularly is so important to assess the health of the tissues in your mouth!
Half of Americans over the age of 30 have gum disease!
https://www.perio.org/consumer/cdc-study.htm
The bone loss that most commonly occurs with gum disease is linear and flat. Imagine the bone surrounding your teeth like a full swimming pool. The water should come up close to the top of the pool. Now picture the water level slowly decreasing, the water level is still flat, but there is not as much as when the pool was full.
Because of this linear and flat pattern of bone loss, regeneration of the bone is just not possible.
In order for the bone to grow and regenerate, it needs to be surrounded by healthy bone with a good blood supply.
There are only certain circumstances where bone can regenerate, for example, when you have a tooth extracted. The socket where the tooth came out of is surrounded by healthy bone and will regenerate to fill the hole.
Again, bone loss occurring from gum disease that has already occurred cannot be reversed and grow back because our bodies are not able to regenerate it. Unfortunately, that is the way our bodies work.
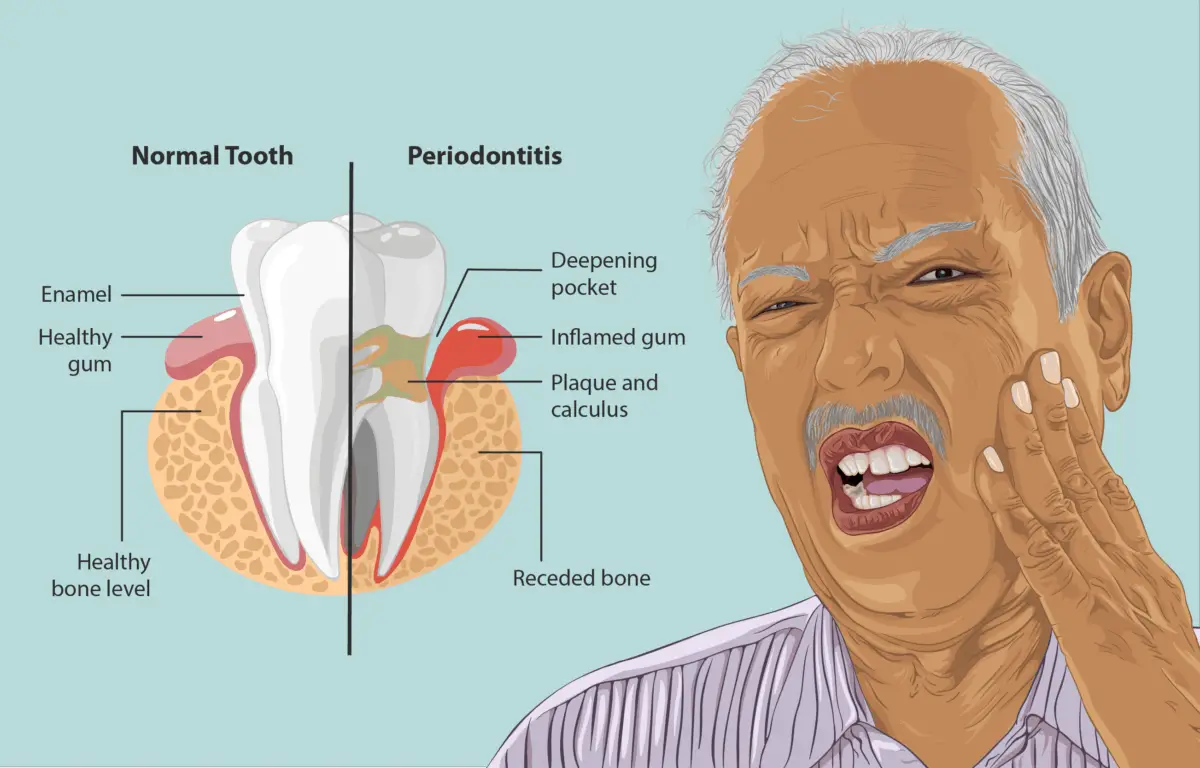
How gum disease causes bone loss in the jaw
Gum disease causes the breakdown of the jaw bone due to being infected by an overload of bacteria. Our body sees the overload of bacteria as an invasion, so our body’s immune system sends out the force of white blood cells to kill off the bacteria and can kill the bone cells in the process.
As well, when the bacteria levels reach a certain threshold, they start to release toxins into the surrounding tissues (gums, bone, and ligaments) of the teeth affected.
When oral hygiene is poor, or you have certain medical conditions or take certain medications/genetic factors that contribute to poor oral health, an infection will start to form in the gums and eventually the bone if not stopped.
Gum disease usually happens at a slow rate, and because of its chronic nature, there is very little to no pain.
Gum disease includes both gingivitis (infection only present in the gum tissue), and periodontitis (infection of the gum tissue, the ligaments surrounding the tooth in the bone socket, and the bone surrounding the teeth and ligaments).

Surgery as a way to maintain bone levels in the jaw
Even though the bone loss in the jaw cannot be reversed, there are some circumstances where surgery can be done or should be done.
Flap surgery (also called pocket reduction surgery) can be performed by a gum specialist/oral surgeon. Flap surgery can be quite successful at reducing the progression of gum disease.
In the post linked below, I go over 14 ways a periodontist will treat gum disease!
Read Now: How Does a Periodontist Treat Gum Disease? Hygienist Explains
Flap surgery is when the gums are flapped open to expose the root surfaces and bone surrounding the teeth to clean the area effectively, remove the tartar (calculus), reshape the bone if needed and remove diseased tissue. In some circumstances, if there is a defect in the bone, a bone graft can be done.
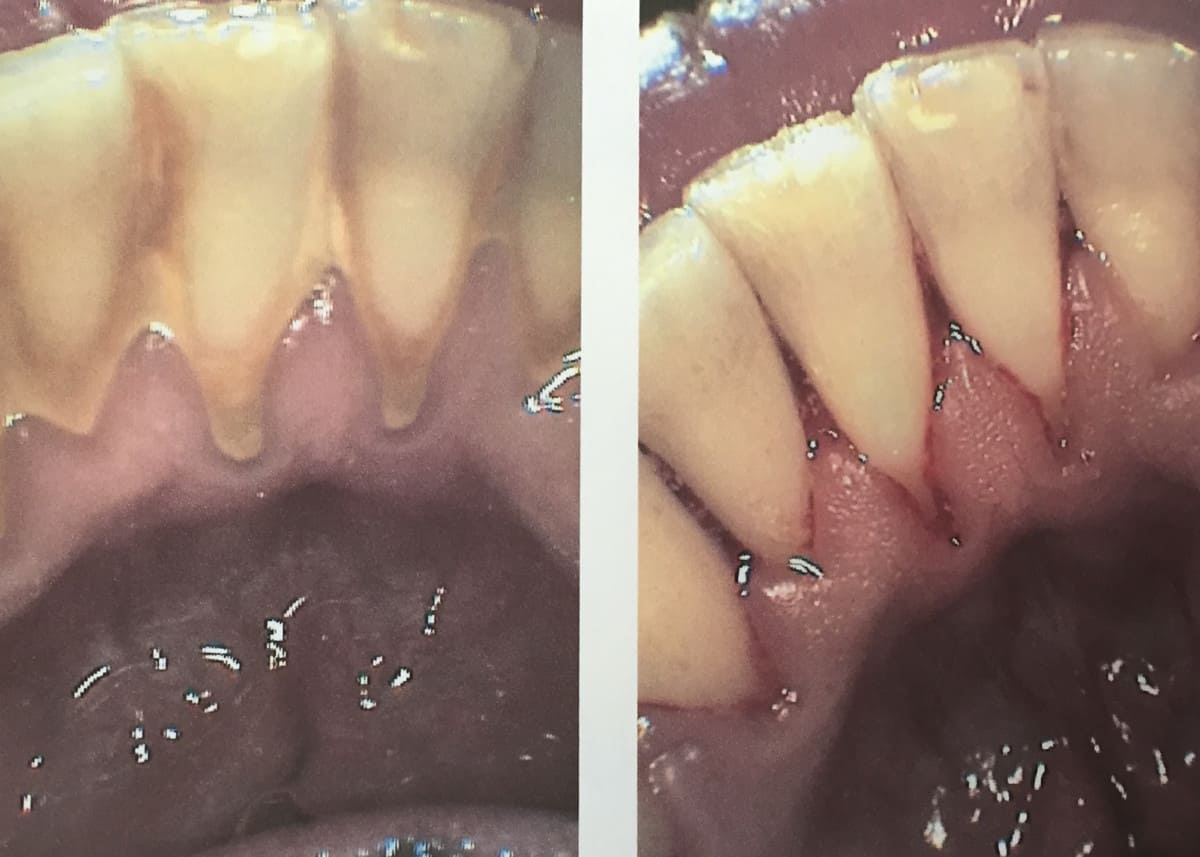
It is good to note that this surgery can cause more recession and make the tooth look longer in the mouth (as you can see in the image above). This is because the aim of the game is to shrink the size of the pocket (to at least 3-4 mm) so it can be cleaned at home effectively.
Read now: Receding Gums? Best Electric Toothbrush and Head to Use!
How quickly does bone loss occur in teeth?
I really dislike answering questions with “it depends” because it really doesn’t give a clear answer. However in this circumstance, “it depends” needs to be used.
The number of risk factors you have determines how fast bone loss can occur in the jawbones. Diabetes, smoking, oral habits, and genetics all have their part to play in the speed of progressing gum disease.
Further along in this post, I have listed 11 causes of bone loss in the jaw.
It also depends on if the bone loss is acute or chronic. This has a major effect on how quickly bone loss will occur.
Chronic vs Acute bone loss *important to know*!!
Chronic bone loss occurs over a long period of time and should not cause any pain because it is so slow. Chronic bone loss is mostly even throughout the mouth, and the bone loss occurs in a flat and linear pattern (remember the swimming pool analogy above?).
Sometimes the chronic bone loss is caused by a missing tooth, as the bone in the jaw needs to be stimulated (by chewing and active forces from the teeth). This is not necessarily a bad thing, as it is not a result of an overload of bacteria.
Gum disease is most commonly a chronic condition however, in more rare circumstances, it can be acute.
Acute bone loss usually occurs over a much shorter period of time, and pain is much more common. Acute bone loss can be extremely destructive to the bone around the teeth in a short period of time. For acute bone loss, it’s commonly more localized to a small area of the mouth.
Because of the destructiveness of acute bone loss, treatment from a dental professional should occur immediately.
Causes/contributing factors of gum disease, causing bone loss in the jaw
Bone loss in the jaw has many contributing factors, and when I am assessing a patient’s oral health status, I take all of them into account. The patient and I work together to see where things can improve, for example, managing the patient’s dry mouth.
Not all of these points will cause bone loss itself but can contribute to the issue. For example, taking an antidepressant medication itself will not cause bone loss, but it can cause dry mouth, which then can lead to a reduction in oral health and therefore contribute to bone loss.
11 Causes/Contributing factors of bone loss in the jaw include;
- Poor oral hygiene
- Smoking
- Medical conditions including diabetes, osteoporosis, heart disease, rheumatoid arthritis
- Medications
- Misaligned teeth and malocclusion (how teeth bite together)
- Trauma/injury
- Infections
- Clenching and grinding teeth
- Poor nutrition
- Genetic factors
- Pregnancy
There are so many contributing factors to bone loss that all affect oral health. The more contributing factors that you tick off, the more likely you will be to develop gum disease.

How is dental bone loss treated and how can it be stopped?
There are many ways to treat bone loss to stop or slow down the spread. It is so crucial for us dental professionals to spread the word and discuss with our patients why stopping the progression of bone loss is important and how it really affects our overall health.
Uncontrolled and progressing gum disease and can play a role in diabetes, Alzheimer’s/cognitive issues, heart disease, rheumatoid arthritis, osteoporosis, adverse pregnancy outcomes, and overall mental health and confidence issues.
Below I go over 6 ways bone loss is treated and things that can help slow the progression of bone loss down.
1. Dental appointments, and consultation with gum specialist (periodontist) to stop the progression of bone loss
Early intervention is KEY, and early intervention happens at the dental office when your oral health is fully assessed. Neglecting your dental visits can lead to long-term issues including the progression of bone loss.
Or if your gums are bleeding, and you notice blood in your saliva after toothbrushing and flossing, it is a sign of inflammation (gingivitis) and possibly periodontitis (when bone loss in the jaw is occurring), and you should see a dental professional.
Seeing a periodontist and forming a treatment plan that is tailored to you, you may be a candidate for oral surgery. Flap surgery (also called pocket-reduction surgery) is a specific surgery to clean more effectively, reduce the depth of your pockets, and shrink the gums.
Flap surgery makes the mouth so much easier to keep clean, can make a significant difference in bone health and can reduce/stop the progression of the disease.
2. Stop/reduce clenching and grinding to stop the progression of bone loss
Because clenching and grinding put extra (unwanted) force and tension on the teeth and bone, it can lead to bone loss. This is how teeth move in the jaw when you have braces on your teeth. The tension/pressure that is caused by the braces, breaks down the bone in the opposite direction of where the pressure is coming from.
Dispersing that force evenly and reducing the wear and tear, can prevent bone loss from occurring.
Personal story:
I am a HUGE clencher, and I have destroyed multiple nightguards (I shudder to think of the damage I could have caused if I never got a nightguard).
When I was younger, a dentist that I used to go to recommended that I get a nightguard, and honestly – between you and I, he really pushed treatment on people and was known for recommending treatment that didn’t need to be done so he could earn money off of it.
I knew this (I still kept going to that office because I loved my hygienist, and I only left after I became a dental hygienist myself). Anyways, long story short, I didn’t end up getting the nightguard that was recommended to me because I didn’t know the benefits of having on or the consequences of not having one.
I didn’t get one until I was a dental hygienist because I became aware of the consequences of clenching and grinding and not wearing a nightguard. And I will never not wear one again!

Splinting teeth together is another option if the bone loss is advanced enough and the teeth are mobile. The teeth are splinted together using dental cement, and commonly a wire/thread to provide stabilization. When the teeth are attached to each other, they will move less and will help to prevent bone loss.
You can see an example of splinting on the bottom front teeth in the image above!
3. Improve oral hygiene habits to stop the progression of bone loss
Assessing oral hygiene habits and how it is done is important to see where it can be improved.
When I am discussing with my patients about their oral hygiene habits, I often touch on things that are often overlooked;
- How often is your toothbrush/toothbrush head changed? Toothbrushes and toothbrush heads should be switched out at least every 3 months, or if the bristles are showing signs of wear before the 3-month mark, or if you are sick.
- Flossing technique
- Wrapping the floss in a “C-shape” around the teeth to get further under the gumline
- Tongue cleaning
- Use of Waterpik
- Electric toothbrush – use one with a visual pressure sensor.
- Interdental brushes
- Time and frequency of oral hygiene
I know I sound like a broken record however, it is so important to see a dental professional, so the recommended oral hygiene routine is 100% tailored to you and your current oral health status.
Especially if you have some limitations such as arthritis or injury that impacts how well oral hygiene can be done.
Below is a video I made to help modify your toothbrush at home if you have mobility issues! 🙂
4. Quitting smoking to stop progression of bone loss
Smoking plays a very large role in gum disease and bone loss progression because smoking affects the healing process in our bodies and affects the microflora in our mouths that contributes to gum disease.
Quitting smoking allows the tissues in the mouth to heal faster and more effectively, therefore, slowing down/stopping the process of bone loss.
If you are interested in reading more about how smoking affects gum disease, here is a study that expands on the topic!
that expands on the topic!
5. See your medical doctor to ensure stabilization of medical conditions (example; diabetes)
Making sure you are in good health can help stabilize gum disease and stop bone loss.
Many different medical conditions that are not under control can speed up the progress of bone loss around the teeth.
For example, uncontrolled diabetes can cause blood sugar levels to rise, which in turn can cause damage to the blood vessels in the body, including in the mouth.
When gum disease progresses and becomes severe, it can raise blood sugar levels in the body, contributing to the destruction of bone and soft tissue surrounding the teeth.
The connection between health conditions and gum disease is rarely talked about (until it’s often too late). It’s really too bad that this information isn’t being talked about regularly. I try to bring up the topic with my patients in my dental chair, even if they don’t have any medical issues.
People who have diabetes are 3X more likely to develop gum disease!
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3228943/#:~:text=It%20is%20highly%20prevalent%20(severe,threefold%20in%20people%20with%20diabetes.
6. Improve nutrition/diet to get the needed vitamins and minerals for gum and bone health
This should be evaluated in conjunction with a medical doctor to ensure that everything taken is safe to use and there is no potential for drug interactions.
But eating well and getting enough vitamins and minerals is crucial to providing your body with the right nutrients to fight off disease and boost the body’s ability to heal. In particular, vitamin D has shown to be a good preventative vitamin to take for gum disease.
Here is a study, “The Role of Vitamins in Oral Health. A Systematic Review and Meta-Analysis “ analyzing vitamins and their effect on the mouth and goes into the finer details.
“ analyzing vitamins and their effect on the mouth and goes into the finer details.
I hope you have found this information useful and informative.
Have a wonderful day, and keep smiling!
Holly 🙂
