As a dental hygienist, I refer my patients to a periodontist when they require extended care. There are multiple reasons why we refer to a periodontist, including dental implant therapy, gum disease evaluation, treatment and therapy, and overall oral health assessment and treatment planning. But specifically, how does a periodontist treat gum disease?
A periodontist treats gum disease by surgically flapping the gum to reveal the jaw bone and tooth surfaces below the gumline. Curettage, bone grafts, gingival grafts, guided tissue regeneration, gingivectomy, crown lengthening, periodontal plastic surgery and frenectomy can help manage the disease.
If gum disease goes untreated, spread of infection, loss of teeth, and need for surgery all increase. That is why I like to refer my patients early on so we can maximize the prevention of gum disease and the effects on our body, such as increased heart disease and inflammatory conditions.
Gum disease (also called oral disease) includes both gingivitis (gums only) and periodontitis (bone and gum involvement) and is a chronic inflammatory condition. Periodontitis is the 6th most prevalent disease in the world.
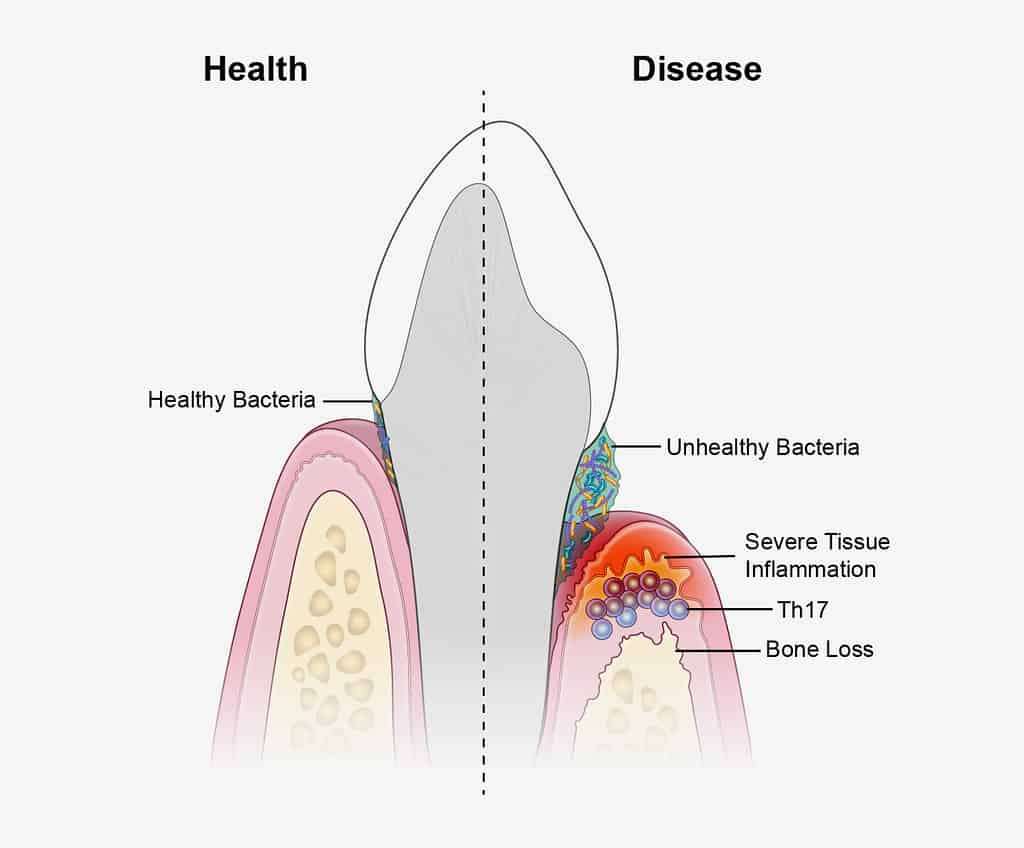
And there is an emerging question in evidence-based science that periodontitis is actually an autoimmune disease. This is really interesting and may start to change how we approach gum disease treatment.
In this post, I briefly cover what periodontitis is, the dental hygienist’s role, and explain different surgeries and treatments that a periodontist may do to treat gum disease.
What is periodontitis and how do you treat it?
Periodontitis is a form of gum disease that involves chronic inflammation of the bone, gum tissue, and ligaments around teeth. Chronic inflammation leads to tissue death, resulting in tooth loss.
Periodontitis is the outcome from the body’s response to bacteria. The body will produce an overactive response to the bacteria in the mouth and create inflammatory cells that kill both infected and healthy tissue. When this process continues without intervention, tissue loss will continue and tooth loss will occur.
How to treat periodontitis usually starts with the dental hygienist. We must assess the gum tissue and bone levels along with cleaning the teeth. We check for areas that gum disease is progressing, at what rate, and how we can adjust our care, and go over oral hygiene routines that will help slow the progression of tissue loss down.
Read Now: How Dental Hygienists Clean Teeth! What You Need to Know!
When the situation is not improving, or it becomes apparent that other interventions will be needed, we refer to a periodontist. In saying so, please ensure that your dental hygienist is measuring your gums (performing a periodontal assessment) regularly.
Below I explain the 14 ways a periodontist treats gum disease.
14 ways a periodontist treats gum disease including surgeries
Sometimes, when seeing a specialist, they don’t fully explain everything to the patient or things are glossed over, leaving the patient with many questions. I often get patients asking me to clarify what has been said or go over it with them again so they can better understand.
Below, I go into detail about all the different types of surgeries that a periodontist will perform when a patient has gum disease.
1. What is gum flap surgery?
To access and treat the structures underneath the gumline, a “flap” is created.
Gum flap surgery is a procedure in which incisions are made in the gum tissue and raised off the teeth to access underlying tooth structures. The tooth surfaces, including the roots of teeth affected by periodontal disease, are treated, and the gum tissue is returned to its original position.
This surgery is more straightforward, only affecting the roots of the teeth, and the tissue is placed back in the original position. Sometimes this gum flap surgery is called “flap for access”.
Read Now: Receding Gums? Best Electric Toothbrush and Head to Use!
However, due to unavoidable circumstances, other styles of flap surgery are performed, including open flap debridement, and placing the gums back in different positions than where they were originally.
2. Open Flap Debridement
Open flap debridement (also termed flap curettage) is similar to flap for access but with a few differences.
Open flap debridement requires more extensive flap elevation, pulling the gum tissue away from the bone more to make more bone visible. More bone tissue and tooth surfaces can be effectively treated.
The gum tissue may be placed back in a different position. Placing the gum tissue back in a different position is done to make it easier for the patient to clean and maintain the area’s health.
3. Apically Positioned Flap
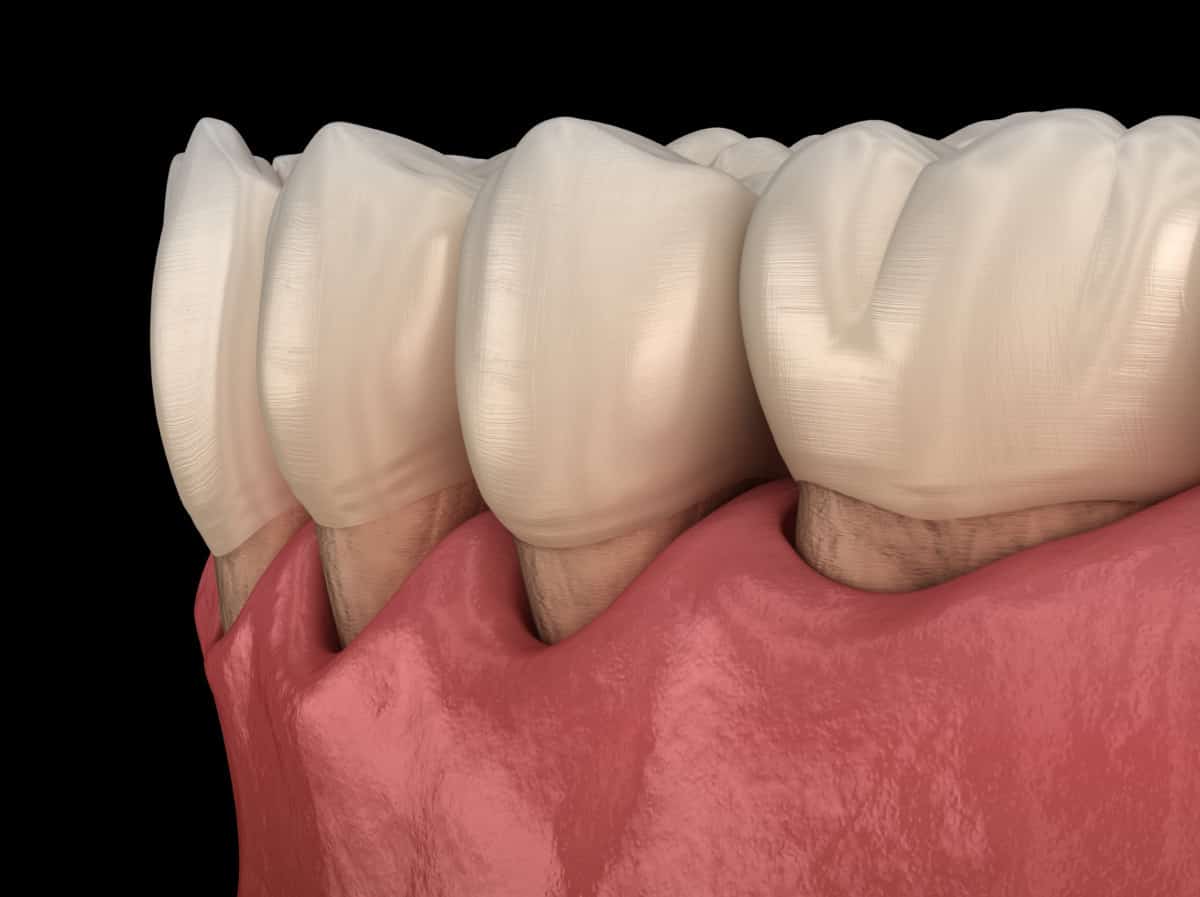
An apically positioned flap is used when bone tissue is being removed. This surgery results in the gum line being lower down (closer to the root tips), causing increased root exposure, reduced pocket depths, and providing access for the patient to clean with a toothbrush and interdental aids.
Although there are benefits to this surgery, the patient needs to be informed of the changes that may occur.
The patient needs to be informed that a portion of the root surface will be exposed, which can lead to cavities on the root surface because the roots are much softer and prone to tooth decay than the crown of the tooth where the enamel is present.
There is also an aesthetic concern. The root surfaces are more yellow than the crown of the tooth and the teeth will appear longer in the mouth. Exposed roots can also lead to more tooth sensitivity.
Even though these aesthetic concerns may bother the patient, doing nothing will exacerbate gum disease and increase the chance of tooth loss.
I tell my patients that I would rather see them with more root exposure and healthier gum tissue than have their gum disease continue to progress!
4. Coronally Positioned Flap
A coronally positioned flap is a plastic surgery procedure that can improve gum recession as long as the recession is not classified as advanced. The flap is relocated higher up on the tooth (closer to the biting surface) to the previous position.
An advantage to this surgery is that it does not need a second surgical site to provide donor tissue. Usually, with gum grafts, tissue is taken from another area of the mouth, such as the palate (called a free gingival graft).
A disadvantage to this surgery is that it can be challenging to stabilize the flap with sutures in a coronal position. The success rate is lower because of the difficulty to manage the height of the gum tissue on the teeth and “hold it in place.”
5. Laterally Positioned Flap
A laterally positioned flap is a plastic surgery technique used to cover root surfaces with gum tissue. This procedure is only used in isolated areas of gum recession.
The tissue from the donor site is lifted and rotated laterally to cover the area of gum recession and provides excellent root coverage. The donor site must be a thick and healthy covering of gum tissue to prevent harm to the donor site.
The laterally positioned flap keeps its blood supply, unlike the free gingival graft (see below for description). Maintaining the blood supply increases the success rate of the graft.
Read Now: Can Bone Loss in the Jaw Be Reversed? Hygienist Explains.
Grafting in the mouth; bone, and gum tissue
6. Bone Replacement Graft
A bone replacement graft is a surgical procedure used to promote the rebuilding of the jaw bone that has been lost due to periodontal disease.
Bone grafts are more challenging in dentistry than in medicine.
Bone grafts cannot usually be done if the bone loss has happened on an even level. Think of the water in a swimming pool evaporating; the water levels will go down evenly. When bone loss in the jaw happens in this way, bone grafts will be extremely difficult and may not even be feasible. A periodontist will assess your situation for bone graft plausibility.
The bone grafts in periodontal defects (where bone loss is uneven) are constantly subjected to contamination from saliva and bacteria. This contamination can occur when bacteria and saliva travel along with the roots beside the bone graft site.
Also, the growth of gum tissue into the wounds can disrupt the healing of the bone graft that can lead to failure.
Meticulous plaque control is critical in maintaining health at the bone graft site and surrounding area of tissue, especially in the months following the bone graft surgery.
7. Periodontal Plastic Surgery
Periodontal plastic surgery is done to correct problems with the gums, improper frenum attachment (where the frenum tissue location between the front teeth is too low, pulling the front teeth apart), or a “gummy smile” is present.
Periodontal plastic surgery can adjust the tissues surrounding natural teeth and dental implants.
Periodontal plastic surgery includes many periodontal surgical procedures used to improve esthetics, enhance prosthetic dentistry, and damage from periodontitis. The main goal is to create a functional, effective, but visually appealing smile.
8. Free Gingival Graft
A free gingival graft is a periodontal plastic surgery procedure. It will Improve the appearance of the tissue, and it is done to prevent further loss of gum tissue that is thinning and at high risk for tissue loss.
A free gingival graft was one of the first procedures used to augment the width of the gum tissue!
This surgery has two sites: the donor site and the recipient site. The tissue harvested from the donor site (usually the palate) includes both surface epithelium and underlying connective tissue to increase the chance of connecting and integrating with the recipient site.
This graft provides root coverage in areas of recession (root exposure). A complicating factor of this surgery is that when the tissue is taken from the donor site, all blood supply is severed, making it all the more important to take special care at the beginning to encourage the diffusion of nutrients to the graft.
During the early stages of healing, taking special care will increase the chance of success.
Other surgeries performed by a periodontist
9. Guided Tissue Regeneration
Guided tissue regeneration is a surgical procedure to encourage the regeneration of tissues in periodontal structures that have been lost.
These structures include cementum (tooth tissue that covers the roots of teeth), jaw bone and periodontal ligament (fibres that hold the tooth to the gum tissue and bone).
The ultimate goal is to have proper regeneration of the periodontium structures. With this surgery, a barrier membrane is placed between the gum tissue and the tissue regeneration site to prevent the gum tissue from quickly growing into the wound.
Delaying gum tissue growth allows undifferentiated cells to populate the root area and develop into cementum, jaw bone and periodontal ligament. If a barrier membrane is not used, the gum tissue will directly contact the wound and prevent the slower growing cells from growing.
10. Frenectomy
A frenectomy is a periodontal plastic surgery procedure that surgically removes the frenum, including the attachment to the bone.
Frenums in the mouth are soft tissue attachments that helps connect the lips to the gums, but sometimes can be too tight.
When the frenum is attached too closely to the gingival margin, it can cause repeated pulling, contributing to persistent inflammation in the tissues and interfere with daily self-care.
An aberrant frenum most commonly affects the frenum between the top and bottom front teeth and is one of the reasons for a gap to form between the front teeth!

11. Crown lengthening surgery on teeth
Crown lengthening surgery is a periodontal plastic surgery that creates a longer clinical crown by removing some of the gum tissue and jaw bone around the necks of the teeth. Crown lengthening is often done to increase the tooth’s surface area to which a dental crown (cap) can adhere.
There are two terms used when describing crown lengthening: functional and esthetic crown lengthening.
Functional crown lengthening is performed when the remaining tooth structure is inadequate to support a restorative dental procedure. Esthetic crown lengthening is done to improve the appearance of teeth, especially on those with short clinical crowns.
In some cases, excess gum tissue covering the teeth may be present and indicated for a crown lengthening surgery. Temporary dentinal hypersensitivity (tooth sensitivity from root exposure) can occur post-surgery.
The dental hygienist is to warn patients in advance that they may experience temporary dentinal hypersensitivity and that meticulous plaque control during the healing phase is critical.

12. Gingivectomy
A gingivectomy is a surgical procedure performed to excise and remove some gum tissue. This surgery results in an apical position of the gum margin and its relationship where the crown transitions to the root. The patient will be able to perform better self-care in those selected sites.
There are some disadvantages of the gingivectomy procedure. The incision made leaves a large area of an open connective tissue wound. Because of this, the healing process is much slower than other surgeries and more discomfort for the patient.
The patient’s teeth will appear longer. Also, a large part of keratinized tissue is not conserved with this procedure which can be inadvisable to remove if it is already of minimal width. The dental hygienist should be aware that the healing phase after this procedure is very uncomfortable and should discuss painkillers with the dentist and patient.
The wound can be managed with a periodontal dressing (bandage). The dressing may need to be changed multiple times until the epithelium has covered the connective tissue completely.
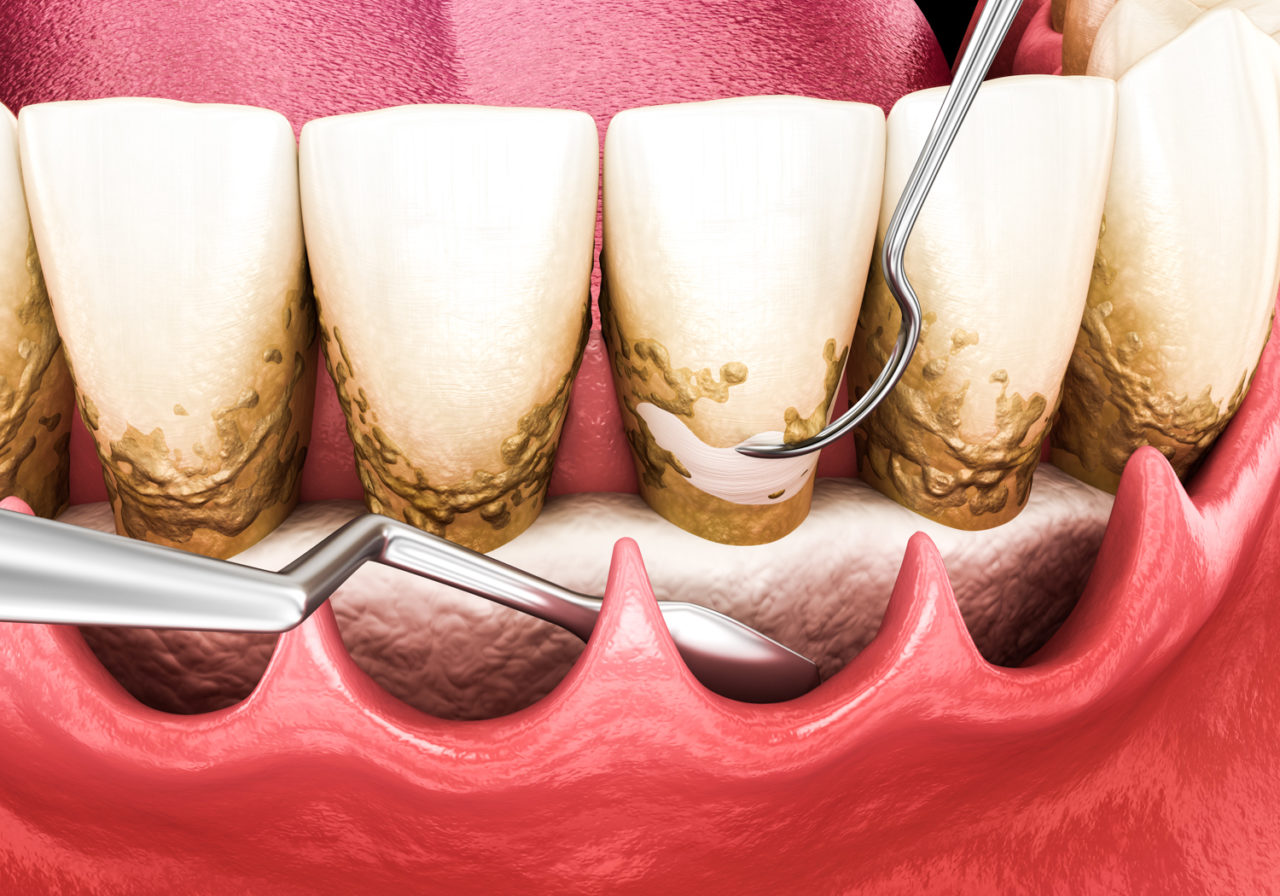
13. Gingival (gum) Curettage
Gingival curettage is an older surgical procedure that involves the intentional attempt to scrape away the lining of the periodontal pocket, usually using a Gracey curet.
It is important to note that studies have shown that the same benefits from gingival curettage can be achieved through periodontal instrumentation and meticulous self-care by the patient.
Because of this, gingival curettage is rarely performed or needed. In some instances, gingival curettage is indicated when more definitive types of surgery are contraindicated because of health concerns in the patient. Also, in sites of persistent inflammation where periodontal surgery has been performed, gingival curettage is effective.

14. Dental implants
I added dental implants to this list, even though they are not really a surgery to treat gum disease. They are a solution to tooth replacement for teeth that have been lost from gum disease.
If teeth have been lost, dental implants are the best treatment to replace the tooth. Dental implants are long-lasting, and do not rely on other teeth such as partial dentures and dental bridges.
However, suppose a patient has more extensive and advancing gum disease. In that case, the periodontist may say that an implant is not possible, or the chance of success is lower than the average.
Controlling gum disease is so crucial before getting implants because the bacteria in the mouth can travel and start to cause destruction around the implant.
If you are looking for more information regarding dental implants, I linked a couple posts below that I wrote that go over dental implant care in much more depth.
Read Now: Dental Implants and How to Take Care of Them After Surgery
Read Now: Dental Implants: Best Way to Clean, Maintain and Care For
Summarized post operatory instructions for periodontal surgery
Post-surgical instructions for the patient are separated into categories of;
- restrictions of self-care
- post-surgical medications
- dietary changes
It is important to remind the patient they can perform regular self-care to those teeth not affected by the surgery. Restrictions of self-care include a prescription of chlorhexidine mouth rinse to use twice daily until the patient can safely resume self-care.
With flap surgery and gingivectomy, self-care can resume in about 10-14 days following.
For other selected periodontal surgeries such as guided tissue regeneration or bone grafting, self-care should be restricted for up to 4 to 6 weeks.
If systemic antibiotics are prescribed, it is important to emphasize that the patient takes all prescribed medications until finished.
The patient should be educated on the importance of a soft or liquid diet for 24-48 hours post-surgery, and chewing should only be done on the side that has not been affected by the surgery. This should be emphasized especially during the early stages of healing.
Instructions for post-surgical complications are given, focusing on facial swelling and post-surgical bleeding. The complication of facial swelling should be discussed with the patient and be told that the facial swelling is common and usually not a sign that healing is compromised. Using ice packs for the first 8 to 10 hours following surgery can help minimize swelling.
It should be explained to the patient that minor bleeding is expected, but if excessive bleeding occurs, the patient should contact the office’s emergency number right away. Patients should be advised that smoking during healing should not be done. Postsurgical visits usually occur within 5 to 7 days after.
Even though this has been a long post, and includes a lot of information, I hope you have found what you were looking for!
Have a wonderful day,
Holly 🙂
Resource – Nield-Gehrig. Foundations of periodontitis for the dental hygienist. 3rd edition. Lippincott, Williams & Wilkins.
